Restoring patient and physician trust in telehealth
3 things that need to happen if telehealth will remain a viable healthcare option post-pandemic—and why they need to
Mahesh Mulumudi, MD
Carmen was a 48-year-old mother of three with diagnosed type 2 diabetes. A single mother, she was working extra shifts to help her youngest attend the nearby state college when she started experiencing shortness of breath and heart palpitations.
Concerned about missing work, Carmen had opted for a virtual doctor’s visit—explaining her symptoms quickly during a ten-minute break in her car. She was diagnosed with anxiety and prescribed a care plan that included a short-term dosage of anxiety medication and follow-up visits with a virtual therapist. Within weeks, Carmen ended up in the emergency department where, upon further examination, it was discovered she had a weak heart pump and was experiencing acute heart failure.
Unfortunately, Carmen’s story is not unique—and it’s instances like this that lead patients and providers alike to remain wary of telehealth.
The loss of trust in healthcare
While a public health crisis has necessitated fast adoption of telehealth, a J.D. Power Telehealth Satisfaction study shares that 43 percent of surveyed patients feel telehealth is cold or “impersonal,” and nearly half believe telehealth offers a lower quality of care than in-person physician visits.
And the lack of confidence goes both ways.
More than ten years after the introduction of Teledoc, arguably the first modern telehealth platform, 75 percent of physicians were still reporting high levels of distrust in telehealth as a viable option for correctly diagnosing a patient. Six years later, the numbers have improved, but only slightly.
Combining better audio-visual capabilities with remote patient monitoring devices can help restore both patient and physician trust in telemedicine’s capacity for long-term, effective value-based care.
Restoring confidence through like-live examinations
Pitfalls of today’s telemedicine system that drive patient and provider distrust include strictly-asynchronous telemedicine models where patient information is submitted for a physician’s later review, or audio-only phone calls where providers lack the opportunity to observe the patient through the addition of live video.
While implementing these “store and forward” or audio-based telemedicine platforms can seem faster to implement than platforms that facilitate live audio-visual telemedicine calls, these models ultimately set both patient and provider up for quick wins rather than reliable, long term gains.
Conversely, a report published by the American Psychiatric Association reviewed 30 randomized controlled trials involving live video-conferencing examinations and found that “With the exception of one study, the review found no statistical difference in clinical outcomes… delivered by synchronous video-conferencing treatment and in-person treatment.”
While it’s easier to see the feasibility of audio-visual calls in addressing mental and behavioral health conditions, these same principles notably improve the quality of care received by chronic care patients as well. When coupled with additional connected devices that offer insight into physical conditions, the visits provided through telehealth services further improve and can even begin to rival the standards of care patients would receive in a traditional clinical visit.
Improving chronic condition care by introducing connected devices into live examinations
Telemedicine as it exists today relies highly on surface level information—things a physician can observe with the eye or be told by a patient—but lacks the ability to observe what’s happening inside the body. As such, evaluating patients through traditional telemedicine practices continues to pose challenges because it still involves a lot of guesswork on the part of the physician—leading to less-confident diagnoses from providers and less confidence in those diagnoses from the patients.
The addition of connected devices—especially for patients with chronic conditions who are seen regularly—can alleviate this guesswork by offering ways for patients to share, and providers to observe, things like heart and lung sounds.
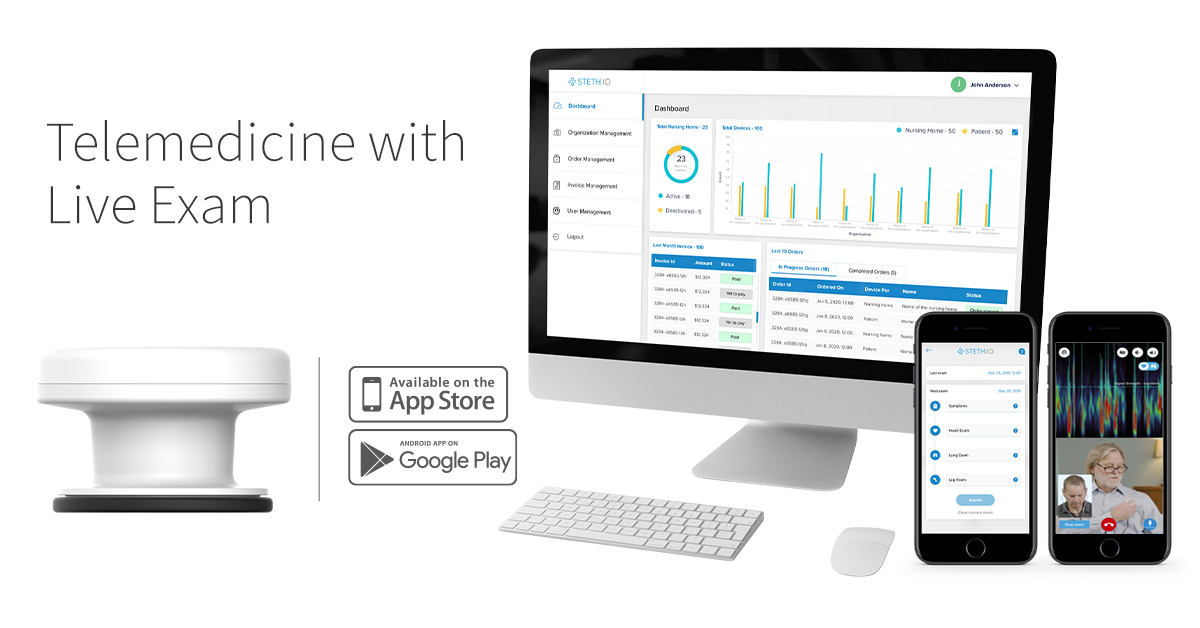
The Steth IO Spot addresses this gap by providing a digital stethoscope that can plug directly into a patient’s smartphone to capture heart and lung sounds as part of a live audio-visual examination via the Steth IO telemedicine platform. As a result, this remote care experience becomes clinical and life-like as patients and providers are able to talk to and see each other while also listening to heart and lung sounds as though the patient was physically in the exam room.
Furthermore, the Steth IO platform augments the telemedicine experience by visually representing sounds from the Spot device on the provider screen—allowing physicians to quickly identify potential issues that would have been more difficult to diagnose by ear alone and triage care accordingly.
For a case like Carmen, having these capabilities upfront could have helped the provider recognize early stages of heart failure more quickly—even at her younger age—and prescribe a more appropriate care plan that would have reduced her risk of needing to be admitted to the hospital.
Providing continued support through ongoing education, reminders, and monitoring
Current patient support functionality, for many healthcare organizations, consists solely of a printed visit summary following an appointment—summarizing what was discussed, outlining expectations, and listing what follow-up the patient needs to take. Where these summaries end, however, the capabilities of telemedicine platforms begin—reestablishing patient trust through better virtual support via telehealth.
In addition to visit summaries, telehealth platforms offer ongoing, comprehensive direction tailored to each patient’s condition and situation in real time. For example, patients can get notifications to take medications, follow their diets, complete daily at-home rehab regimens and schedule their five-day follow-up appointments—all within one app.
For telemedicine platforms like Steth IO that are able to combine live audio-visual visits with remote patient monitoring within a single platform that also offers post-exam support, patient experience is both simplified and improved. As a result, the comprehensive support provided—which would not have been possible through a clinical visit alone—leads to better patient trust and better overall outcomes.
The bottom-line benefits of telemedicine
The long-term benefits that telemedicine can offer patients with chronic conditions far outweigh the initial cost of platform integration, but only when we’re willing to commit the time and resources upfront to following best practices and establishing models that help both patients and their providers feel confident in the technology. When this is achieved, patient health outcomes and quality of life improve—as do care costs over time.
It has been proven that audio-visual visits achieve average short-term cost reductions between $19-$121 per visit in cost avoidance—and larger long-term savings as patients avoid unnecessary emergency and inpatient utilization, readmissions, and more. Furthermore, as we improve the quality of our virtual visits through platforms like Steth IO, we can reduce the pressure providers feel to order extra and unnecessary tests—a large source of unnecessary cost to both patient and payers—that overcompensate for lack of confidence in the diagnosis as a result from poor telehealth platforms.
As we continue to fine-tune our telehealth capabilities, telemedicine platforms like Steth IO will become a key player in affordably improving patient care as we move past the pandemic and into a healthcare system that is increasingly more focused on value-based models of care.
